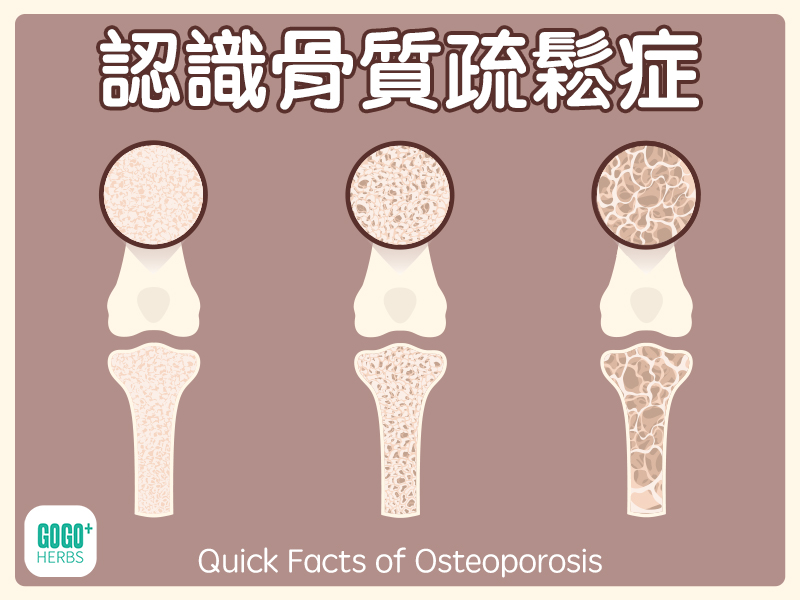
Understanding Osteoporosis
Osteoporosis and related fractures are becoming increasingly common in Taiwan. The book *Mayo Clinic on Osteoporosis*, published by CommonWealth Publishing, explains the causes, prevention, and treatment of osteoporosis in a clear and accessible way, providing readers with practical health information. The following are excerpts of key points from the book for readers' reference.
Diagnosis of osteoporosis: Bone mineral density measurement
"Are my bones healthy? Do I already have osteoporosis?" Bone densitometry is an important tool for diagnosing osteoporosis. It can detect osteoporosis or osteopenia early, which means that bone density is lower than normal, but has not yet reached the standard for osteoporosis.
Based on physician recommendations, the following groups should undergo bone mineral density testing:
Women under the age of 65: Early detection is key.Bone lossCondition.
For individuals aged 40 and older who have experienced a fracture: Assess fracture risk and consider treatment.
High-risk groups for osteoporosis: Those who meet two or more of the following criteria:
Those who are currently taking or about to take corticosteroid medications.
Those with low levels of estrogen or testosterone.
People with diseases that affect bone density or increase the risk of fractures.
Premenopausal women: Consider testing before age 50 (menopause).
High-risk groups or those who have had fractures: It is recommended to get tested as early as possible.
Postmenopausal women who have experienced a fracture: Assess the rate of bone loss and the severity of the disease.
Bone mineral density (BMD) testing is usually not a one-time examination. Even if the initial test results are normal, it is recommended to have a follow-up examination every 5 years to monitor the rate of bone loss over the long term. The frequency of follow-up examinations will be adjusted according to age and risk factors. Significant changes in bone mineral density usually take 1-2 years to become apparent. For those taking osteoporosis medications, it is recommended to have an annual test for the first 1-2 years, and then adjust the frequency of testing after bone mineral density stabilizes. For those taking corticosteroids, annual testing is recommended.
Selection of bone mineral density testing methods
The choice of bone mineral density testing method depends on age, purpose of testing, and risk factors:
Low-risk groups: Consider starting with lower-priced peripheral screening tests (such as pDEXA or pQUS). If the results show...Bone densityIf the value is too low, a more precise central bone mineral density (DEXA) measurement should be performed.
High-risk groups or those who have had a fracture: DEXA testing is recommended directly. For women under 65 years of age, spinal testing is recommended; for women over 65 years of age, hip testing is recommended.
Secondary osteoporosis: Doctors will choose the testing method based on the underlying cause of bone loss. For example, patients with hyperparathyroidism are advised to have their forearm bones tested.
For those diagnosed with osteoporosis: Regular DEXA testing is recommended to assess bone density in fracture-prone areas such as the hip, spine, and wrist. It is advised that the same technician use the same instrument to test the same bones to ensure accurate results.
For those monitoring the effectiveness of medications: It is recommended that those taking medications such as bisphosphonates or teriparatide have their spinal bone mineral density tested.
Diet and Bone Health
Preventing and treating osteoporosis requires a multi-pronged approach, including a balanced diet, regular exercise, healthy lifestyle habits, and appropriate medication. A balanced diet should include sufficient calcium, vitamin D, and other nutrients. Calcium and vitamin D are key nutrients for maintaining bone density. Minerals such as protein, phosphorus, sodium, and magnesium also play important roles.
To increase calcium intake, it is recommended to obtain it from food. Milk and dairy products are good sources of calcium; choose low-fat or skim dairy products. If dietary calcium intake is insufficient, consider calcium supplements. Common calcium compounds include calcium carbonate, calcium citrate, and calcium phosphate. When choosing calcium supplements, consider absorption rate and personal preference. Calcium carbonate is cheaper but may cause constipation; calcium citrate has a high absorption rate but a lower calcium content; calcium phosphate is less likely to cause constipation.
Calcium supplementation recommendations:
Read the product label carefully, paying attention to the calcium ion content and dosage.
Take in divided doses, each dose not exceeding 500 mg.
Take it with food to improve absorption.
Choose products with the USP mark.
Avoid products containing ingredients such as oyster shells, bone meal, or dolomite.
Use pillboxes to track dosage.
Do not consume more than 2500 mg per day.
Calcium supplements may cause side effects such as bloating, abdominal distension, and constipation. It is recommended to drink plenty of water, exercise regularly, and eat more fruits, vegetables, and whole grains to reduce these side effects. If discomfort occurs, you can try a different calcium supplement with different ingredients. In short, the prevention and treatment of osteoporosis requires a long-term and comprehensive strategy; a balanced diet, regular exercise, and regular bone density testing are key. If you have any questions, consult a professional physician.
Related Post:
Related Products:
-
Jamieson – Calcium Concentrate 650mg + Vitamin D3 400IU 120 capsules
Original price was: $108.00.$88.00Current price: $ 88.00. Add to basket -
caltrate – Calcium 600mg + Vitamin D3 800IU & Minerals (Value Pack) 176 capsules
Original price was: $198.00.$180.00Current price is: $180.00. Add to basket -
Jamieson – Vitamin D3 1000IU 375 Capsules 2-pack
Original price was: $180.00.$148.00Current price is: $148.00. Add to basket